CBCT in Implant Dentistry
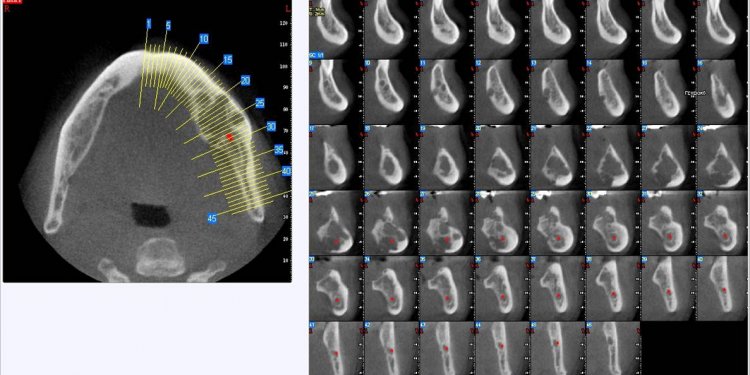
Cone beam computed tomography (CBCT) scanners for the oral and maxillofacial region were pioneered in the late 1990s independently by Arai et al. in Japan and Mozzo et al. CBCT has a lower dose of radiation, minimal metal artifacts, reduced costs, easier accessibility, and easier handling than multislice computed tomography (MSCT); however, the latter is still considered a better choice for the analysis of bone density using a Hounsfield unit (HU) scale. Oral implants require localized area of oral and maxillofacial area for radiation exposure; so, CBCT is an ideal choice. CBCT scans help in the planning of oral implants; they enable measurement of the distance between the alveolar crest and mandibular canal to avoid impingement of inferior alveolar nerve, avoid perforation of the mandibular posterior lingual undercut, and assess the density and quality of bone, and help in planning of the oral implant in the maxilla with special attention to the nasopalatine canal and maxillary sinus. Hence, CBCT reduces the overall exposure to radiation.
Keywords: Cone beam computed tomography, Hounsfield units, multislice computed tomography
INTRODUCTION
Cone beam computed tomography (CBCT) was introduced to the dental field to replace the cumbersome, expensive, and high-radiation–producing medical CT scans around a decade ago Suomalainen et al. found that the CBCT scans were more accurate than CT scans. The American Association of Oral and Maxillofacial Radiology has stated that cross-sectional views are recommended for planning dental implants, and this in combination with the easy accessibility, easy handling, and low-radiation dose of CBCT imaging will lead to the widespread use of CBCT imaging in implantology. Considering the dose of radiation from other image acquisition modalities such as multislice computed tomography (MSCT, e.g., MaxMand CT scan: Effective dose of 2100 according to the 1990 recommendations of the International Commission on Radiological Protection (ICRP)) and panoramic radiography (e.g., panoramic OrthoPhos Plus: Effective dose of 6.3 and 13.3 according to ICRP 1990 and 2005, respectively), CBCT has lesser radiation than MSCT and 10 times more radiation than a panoramic X-ray. The dose of radiation should be reported in millisievert (mSv) or microsievert (μSv) to express the effective dose (E). As Ludlow stated, the E of radiation has been recommended by the ICRP as a means of comparing the detriment of different exposures to ionizing radiation to an equivalent detriment produced by a full-body dose of radiation. The E should be calculated using the equation E = PwT_HT, where wT = weighting factor, HT = equivalent dose. The HT should be calculated using the equation HT = PwR_DT, where wR = radiation weighting factor (which is 1 in the case of X-ray radiation), DT = absorbed dose. Benefits of CBCT are three-dimensional (3D) dataset, real-size data, the potential for generating all 2D images (e.g., orthopantomogram, lateral cephalogram, imaging of the temporomandibular joint (TMJ)), potential for vertical scanning in a natural seated position, isotropic voxel size, high-resolution (e.g., bone trabeculae, periodontal ligament (PDL), root formation) imaging, lower dose of radiation than MSCT, less disturbance from metal artifacts, reduced costs compared with MSCT, easier accessibility, in-office imaging, easier handling, small footprint, Digital Imaging and Communications in Medicine (DICOM) compatiblity, user-friendly postprocessing and viewing software, and better saving of energy compared with MSCT. Limitations are low contrast range, limited detector size causing limited field of view and limited scanned volume, limited inner soft tissue information, increased noise from scatter radiation and concomitant loss of contrast resolution, movement of artifacts affecting the whole dataset, truncation artifacts (caused by the fact that projections acquired with the region of interest selection do not contain the entire object), and that they cannot be used for estimation of Hounsfield units (HUs). HUs represent the relative density of body tissues according to a calibrated...